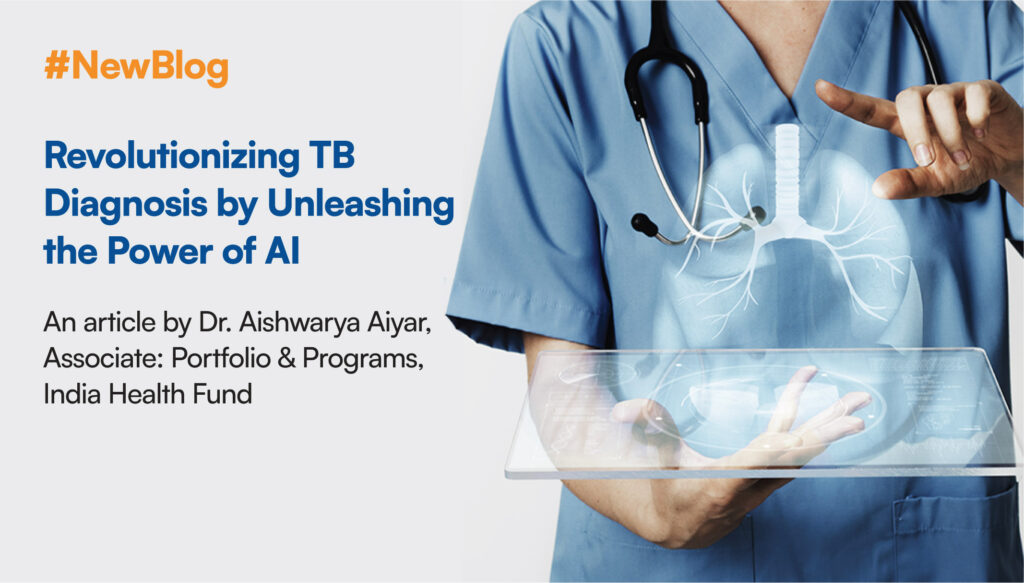
Infectious diseases continue to be a major public health concern, particularly in developing nations like India where they are the leading causes of mortality, morbidity, and disability. The World Health Organization (WHO) estimates that India contributes to more than a quarter of the world’s 10 million tuberculosis (TB) cases.[1] Close to 505,000 people died from tuberculosis in 2021 in India, a substantial 10% increase from the previous year[2]. Delayed diagnosis, lack of rapid, sensitive, accurate and portable diagnostics, manual errors in interpretation of tests, insufficient training of workforce to use these advanced tests, and expense incurred in the procurement & maintenance of these equipments are a few challenges in the current TB diagnostics spectrum that contribute significantly to India’s outsized TB burden.
Early diagnosis of TB could be a game-changer that can save millions of lives. The WHO estimates that each year, approximately 3 million cases of TB are missed or go untreated globally. [3] These “missing millions” of TB-affected people who are neither detected nor treated, result in worse outcomes, more TB exposures[4] and may result in continued transmission of this potentially fatal disease by acting as community reservoirs of the TB bacterium. Part of the reason for the missing millions are screening and diagnostic gaps in the current TB care cascade. Ranging from the plight of an individual who must wait for weeks to get a laboratory report, to individuals who may not have access to TB diagnostic tests, to people who may not seek care owing to the socio-demographic variables and myths around TB, to those patients who fail to be diagnosed despite reaching health facilities due to lack of diagnostic facilities or the absence of trained laboratory technicians and pulmonologists to detect and treat the condition.
The efficacy of culture-based TB diagnosis, which has been considered the gold standard[5] in clinical practice, is hindered by high test turnaround times. To address this, MTB/RIF assays like GeneXpert and Truenat[6] which are semiautomated rapid molecular testing methods for identifying Mycobacterium tuberculosis DNA and resistance to the drug rifampicin were developed. However, as of 2022, their application continues to be far too restricted with only 1.9 million (33%) people taking it as an initial diagnostic test worldwide.[7] Although GeneXpert and Truenat still remain the primary testing mechanisms for TB, the healthcare sector is proactively looking for alternatives to address these issues of limited test menus, high cost, low throughput, sample type limitations, and dependencies such as electricity and trained human personnel. To fill these gaps and improve diagnostic competencies, more recent technologies are being developed.
One that holds tremendous potential of transforming the infectious disease diagnosis landscape is artificial intelligence (AI) along with other adjunct technologies like machine learning. Researchers and innovators are utilizing the power of AI to supplement and enhance the current diagnostic methods in recognition of the need for increased accessibility, cost-effectiveness, sensitivity, awareness, and infrastructure. Who would have thought that TB diagnosis could be done within minutes using artificial intelligence by analyzing a chest X-Ray with a smartphone? Or that one can diagnose a condition like TB using sound analytics? But both are a reality now! AI algorithms are now being trained to analyze medical images, cough patterns, and vocal tones, with a level of accuracy that is comparable to that of human radiologists.[8]